The Most Important Hole in the Skull You Are Not Thinking About
The Most Important Hole in the Skull You Are Not Thinking About
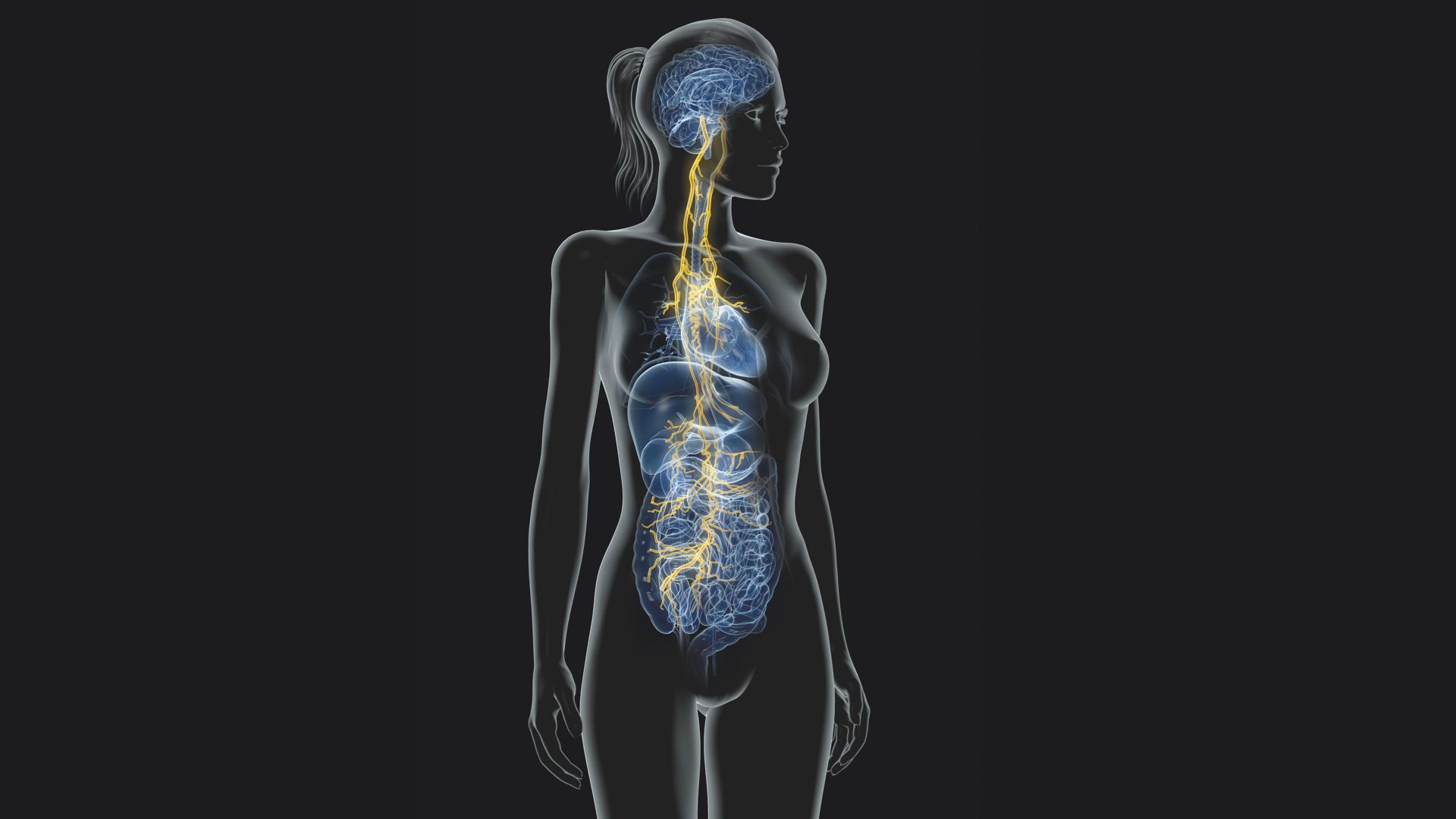
The jugular foramen sits at the junction of the occipital and temporal bones, immediately adjacent to the occiput-atlas articulation. Through it passes the vagus nerve, the glossopharyngeal nerve, and the spinal accessory nerve. The vagus and spinal accessory nerves share a large posterior adipose column within the intraforaminal extradural neural axis compartment, separated from the glossopharyngeal nerve by a fibrovenous curtain of meningeal dura.
This is not an academic anatomy detail. It is the structural reason why upper cervical dysfunction has autonomic consequences that most practitioners either miss or attribute to something else entirely.
Two Mechanisms, Not One
When a positive PRYT pattern creates chronic fascial tension and hypertonic suboccipital musculature in the neighborhood of the jugular foramen, two separate things are happening to the vagus nerve simultaneously.
The first is physical. Sustained mechanical tension from a fixation pattern, fascial restriction from chronically hypertonic suboccipital musculature, or postural strain from a positive yaw 1 or pitch extension pattern can all create low-grade compression on the vagus as it exits the skull. Decreased elasticity in the sternocleidomastoid, documented in the research literature, can restrict vagal nerve movement and predispose to entrapment with downstream neuroinflammation. The rectus capitis lateralis runs immediately anterior to the neurovascular structures at the jugular foramen level. This is tissue you are directly addressing with PRYT examination and correction.
Physical entrapment does not require gross pathology. It requires only the chronic, low-level tissue tension that accompanies a subclinical fixation pattern. That is precisely the clinical population you are working with.
The second mechanism is neurological and may be more clinically significant.
The NTS Is Not a Relay Station
The nucleus tractus solitarius occupies the dorsomedial medulla oblongata. It is the primary termination site for vagal afferent fibers arriving from the heart, lungs, great vessels, esophagus, stomach, small intestine, and proximal colon. It also receives input from the glossopharyngeal nerve, the trigeminal nucleus, and from upper cervical spinal cord levels via the spinosolitary tract.
The NTS does not simply relay information. It functions as a comparator, evaluating error signals between descending neural projections and cardiovascular receptor afferents, then projecting to nuclei that regulate circulatory variables. It modulates the gain of vagal reflexes. It regulates gastric secretion and motility through glutamatergic transmission to the dorsal motor nucleus of the vagus. It coordinates respiratory rhythm through connections with the pre-Botzinger complex. It communicates bidirectionally with the hypothalamus and limbic system through the central autonomic network.
Different vagal populations project to specific NTS subnuclei with differential termination patterns. TRPV1-expressing afferents terminate in medial regions near the caudal obex. 5-HT3 positive afferents terminate in ventral and lateral regions throughout the rostral-caudal medulla. This organization means different visceral functions are regulated through anatomically distinct circuits within the same nucleus.
A disruption in the NTS neighborhood does not produce one uniform autonomic effect. It produces a pattern of effects depending on which circuits are most affected by the incoming noise.
Why Your Post-Correction Findings Vary Between Patients
This is the explanation for the clinical variability you observe after upper cervical PRYT correction. Some patients show ICV tone changes. Some show blood pressure normalization. Some show gastric pattern shifts. Some show respiratory changes. Some show combinations of all of these.
You are not producing one effect. You are improving signal quality in a neighborhood where multiple specific circuits are running simultaneously, each with its own subnuclei termination pattern. The pattern of improvement reflects which circuits were most affected by the chronic dysregulation in that particular patient.
Upper cervical proprioceptive input arrives into this regulatory environment continuously via the spinosolitary tract. In a normally functioning system, that input is part of the sensory context the NTS uses to calibrate autonomic reflex gain across all of those circuits. In a system with chronic upper cervical fixation patterns, that input is dysregulated, excessive, or temporally disordered. The NTS is receiving noise from one of its primary input channels and integrating that noise into regulatory output across multiple visceral systems simultaneously.
This is not a compression story. It is a signal quality story. And it is sitting upstream of every autonomic finding in your recheck.
The Research Confirms It
Post-isometric muscle energy techniques applied to the upper cervical spine at the OA, AA, and C2 levels produce statistically significant increases in RMSSD, pNN50, and high-frequency HRV power. Parasympathetic tone measurably shifts after upper cervical correction. This is not theoretical. These are measured autonomic parameters responding to the same joint levels you are addressing with PRYT.
Manual cervical correction produces concurrent reductions in both systolic and diastolic blood pressure through documented autonomic modulation. The mechanism appears to involve decreased sympathetic influence and activation of the parasympathetic nervous system, confirmed by shifts in HRV parameters toward parasympathetic dominance.
When you find a positive pitch, yaw 1, or tilt pattern and correct it, you have changed the mechanical environment at the jugular foramen and changed the signal quality feeding the NTS. Both mechanisms are operating simultaneously. Your recheck is not confirmation that you did something. It is measurement of a systemic autonomic shift that happened the moment you resolved the fixation.
Apply
After every upper cervical PRYT correction, recheck ICV tone. Recheck hiatal hernia patterns. Recheck inspiration and expiration faults. Check blood pressure if you have the equipment. Assess heart rate variability if you can measure it.
Also notice the spinal accessory nerve. When you find SCM and trapezius tone abnormalities in a patient who also has autonomic findings, remember that the spinal accessory nerve shares a dural compartment with the vagus at the jugular foramen. They are anatomical neighbors. The tone problem and the autonomic problem may share a common mechanical cause that your PRYT correction just addressed.
The next piece covers the finding that reframes everything above it. The myodural bridge is a direct structural connection between your suboccipital corrections and the dural system, and the research on what it does to CSF dynamics changes how you think about every chronic case you have been unable to fully resolve.
Not a member of the weekly focus?
Join us for the deep dives and all the content of the fundamental Applied Kinesiology course inside the monthly membership of Applied Kinesiology Online!
Cant wait to see you inside of this game we call practice!

