The Structure Nobody Taught You About Is Running Between Your Correction and the Dura
There is a dense fibrous connective tissue structure connecting the suboccipital musculature directly to the spinal dura mater. It passes through the posterior atlanto-occipital and atlanto-axial interspaces. Its fibers consist primarily of type I collagen arranged in parallel orientation, designed specifically to transmit strong tensional forces from muscle contractions to the dural sheath. It is called the myodural bridge complex, and it changes the scope of what you are doing with every upper cervical PRYT correction.
This is not a newly theorized anatomical relationship. It is a documented structure with known mechanical properties, known sensory receptor populations embedded within its own fibers, and measured effects on CSF dynamics. The research on it is recent enough that most practitioners have never encountered it in any formal training context.
One Tissue System, Not Three
The posterior atlanto-occipital membrane, the atlanto-axial membrane, and the dura mater develop from a common mesenchymal origin. Between weeks 11 and 14 of fetal development, dense fibrous connective tissue connections progressively integrate from multiple suboccipital muscles, including the rectus capitis posterior minor and major and the obliquus capitis inferior, directly into the dura.
They are not separate structures that happen to be adjacent. They share a developmental lineage and form a functional continuum.
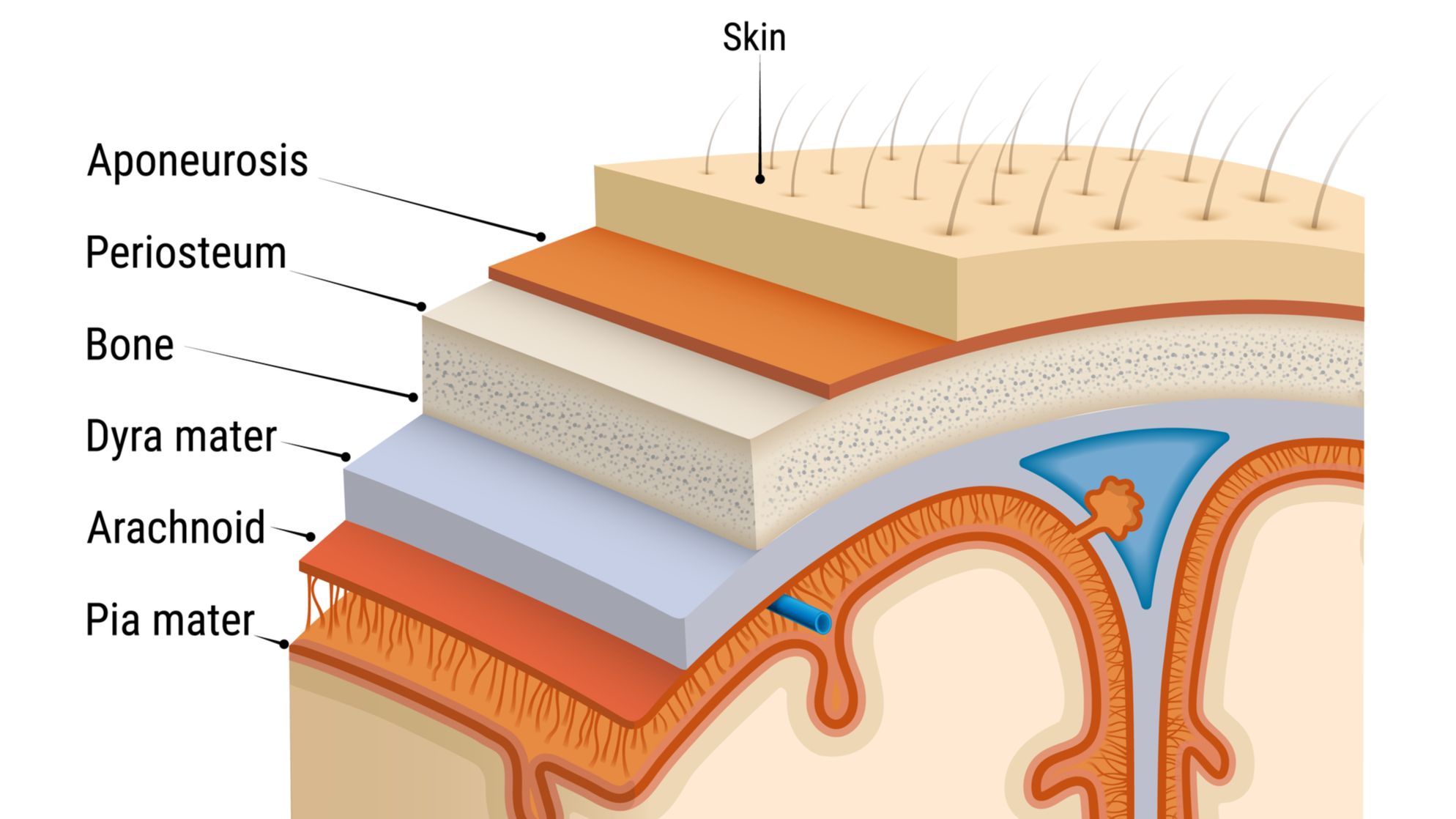
This means fixation patterns at the occiput-atlas-axis complex are not just joint problems. They are not just proprioceptive input problems. They are problems in a continuous tissue system that includes the dura itself. The atlanto-dural and axio-dural ligaments extend from the posterior arch of C1 and the lamina of C2 directly to the dura, creating a thickened dural region at the C1-C2 level. The vertebrodural ligament links the posterior atlas-axis region to the dural sleeve. These are the structural reasons why atlas and axis fixation patterns have consequences that extend beyond any joint capsule.
The Bridge Is a Sensory Organ
The myodural bridge is not just transmitting mechanical force to the dura. It contains four types of sensory receptors embedded within its own fibers: Ruffini corpuscles distributed perivascularly, Pacinian corpuscles located near the dura and muscle attachments, Golgi-Mazzoni corpuscles, and widely distributed free nerve endings.
The bridge is itself a proprioceptive organ participating in the same sensory signaling network you are addressing with PRYT. It is monitoring position and movement at the craniocervical junction and feeding that information back into the system. When the bridge is under chronic abnormal tension from a fixation pattern, it is not a passive victim of that dysfunction. It is an active sensory participant generating dysregulated input from within the bridge tissue itself.
The CSF Pump
The myodural bridge functions as a physiological pump for cerebrospinal fluid circulation. Head movement generates mechanical forces transmitted through the bridge to the dura, creating pressure waves that facilitate CSF movement through the craniocervical junction.
The research is direct. Electrical stimulation of the obliquus capitis inferior, a muscle you address with PRYT correction, produced measurable CSF pressure increases at multiple intracranial locations. The occipital pole showed the earliest pressure response, with waves propagating through the subarachnoid space and ventricles. Head rotation transmitted through the myodural bridge increased maximum CSF flow rates and stroke volumes during ventricular diastole.
Suboccipital muscle function directly influences CSF secretion rates and intracranial pressure. Hyperplasia of suboccipital muscles increased CSF secretion rates and intracranial pressure significantly. Surgical severance of the bridge decreased intracranial pressure. The mechanical coupling between suboccipital muscle function and CSF dynamics is not theoretical. It is measured and directional.
What Chronic Fixation Actually Does
Here is where the clinical picture becomes sobering for long-term cases.
When the myodural bridge undergoes compensatory hyperplasia in response to reduced compliance of surrounding structures, collagen fiber density increases significantly. This further restricts CSF flow through the craniocervical junction. Chronic upper cervical fixation patterns are not just neurologically disruptive in the moment. They may be progressively altering the mechanical properties of a dural system that drives CSF circulation through the craniocervical junction over time.
The sphenobasilar fault patterns and inspiration-expiration faults you recheck after PRYT correction are not incidental findings sitting beside your upper cervical work. They may be downstream expressions of a dural mechanical system that your correction just changed. Flexion and extension faults at the sphenobasilar junction, cranial rhythmic impulse irregularities, chronic upper cervical tension that never fully resolves with standard care. All of it potentially connected to a dural pump mechanism that has been mechanically compromised by the same fixation pattern you are clearing with PRYT.
Apply
When you correct a positive upper cervical PRYT pattern, you are not just resetting spindle tone. You are not just improving proprioceptive input to the cerebellar comparator. You are not just changing the mechanical environment at the jugular foramen. You are changing the tension state of a dural system that is embryologically continuous with the tissue you just corrected, and you are altering the mechanical efficiency of a CSF pump that depends on normal suboccipital muscle function to operate.
Recheck the sphenobasilar junction after your upper cervical PRYT corrections. Recheck cranial findings that seemed unrelated to the presenting complaint. Document what changes. In chronic cases that have been partially responsive to standard care, the myodural bridge may be the missing piece explaining why the correction does not hold and why the dural findings keep returning.
Goodheart built this system by observing what happened clinically and working backward to the mechanism. The research has now caught up to what he was seeing. The mechanism was always there. We just have the language for it now.
Not a member of the weekly focus?
Join us for the deep dives and all the content of the fundamental Applied Kinesiology course inside the monthly membership of Applied Kinesiology Online!
Cant wait to see you inside of this game we call practice!

