Your Neck Muscles Are Not Doing What You Think They Are
There is a small cluster of muscles at the base of your skull that contains up to 500 neuromuscular spindle cells per gram of tissue. The large paraspinal muscles of your lumbar spine contain roughly 3 to 5. Your quadriceps, responsible for extending the knee against significant load, contain fewer still.
The suboccipital muscles were never designed to be prime movers. They are sensory transducers, and the signal they generate continuously is feeding some of the most consequential neurological integration in the human body. Every PRYT correction you make is working directly on this tissue. The clinical results you see afterward are not coincidental findings. They are mechanistically predictable once you understand what this tissue is actually connected to.
Two Signals, Multiple Destinations
Inside each muscle spindle, intrafusal fibers are innervated by two types of afferent neurons. The Ia fibers wrap around the nuclear bag and chain fibers as primary annulospiral endings. They respond to both the rate of change of muscle length and its absolute length simultaneously, making them exquisitely sensitive to dynamic stretch. They are not simply reporting position. They are reporting the quality and dynamics of movement as it unfolds in real time.
The Ib fibers innervate the Golgi tendon organs sitting in series with the muscle at the musculotendinous junction. They encode tension, not length. When contractile force rises, Ib firing increases, activating inhibitory interneurons in the dorsal horn that suppress alpha motor neuron drive to the agonist and facilitate the antagonist. This is autogenic inhibition, and it is the mechanism you are recruiting during PRYT corrections when you resist your patient's maximal isometric contraction.
But here is where the standard explanation requires updating.
Recent evidence shows that GTO-driven autogenic inhibition is transient. The inhibitory effect lasts only as long as the active contraction itself. It does not account for the prolonged range of motion changes and tone shifts you observe clinically after a PRYT correction. The Ib pathway is also context-dependent. During different movement conditions, inhibitory Ib pathways can become excitatory. You are not producing a simple fixed suppression of motor output. You are reconfiguring the reflex pathway itself based on the movement context you created.
Gamma motor neurons are the efferent arm of spindle sensitivity regulation. They innervate the intrafusal fibers and set the mechanical sensitivity of the spindle. After a maximal isometric contraction, gamma motor neuron activity does not simply return to baseline. It undergoes complex re-tuning that changes the threshold for subsequent stretch reflex activation. The spindle establishes new operating parameters.
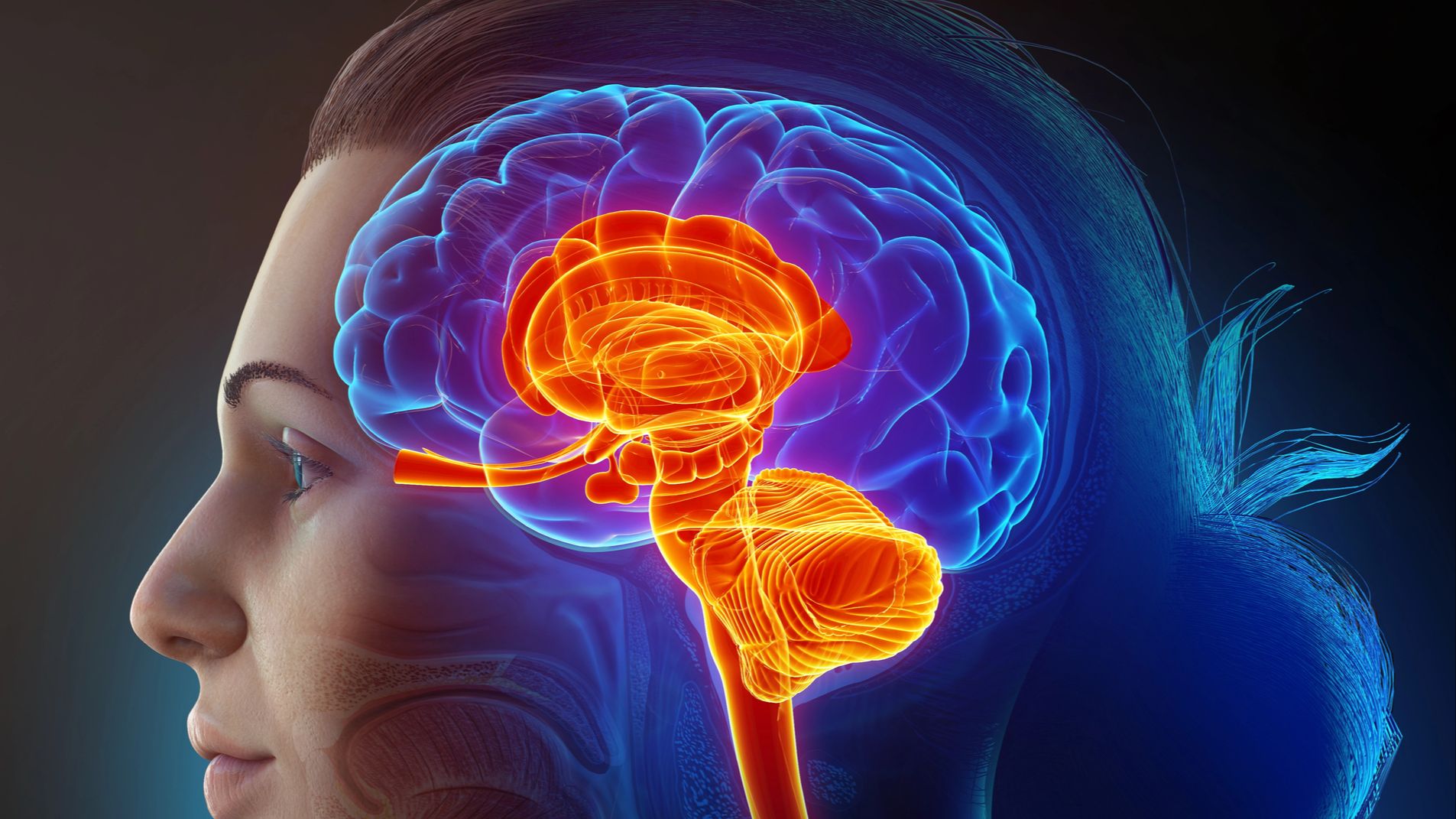
In the suboccipital musculature, this Ia and Ib signaling feeds simultaneously into the spinocerebellar tracts, the vestibular nuclei, the trigeminal sensory complex, and through the spinosolitary tract, directly into the brainstem autonomic regulatory neighborhood. The spindle density means the signal-to-noise ratio from this tissue is extraordinarily high. When that signal is corrupted by a fixation pattern, you are introducing systematic error into multiple integration systems at once. When you correct it, the lasting clinical effect is the downstream recalibration of those systems.
The Cerebellar Comparator
The cerebellum operates as a predictive comparator. It receives efference copies of motor commands from the cortex, then compares intended movement against actual sensory feedback arriving via the spinocerebellar tracts. Discrepancies generate error signals processed through the deep cerebellar nuclei and sent back through the thalamus to the motor cortex and directly to the red nucleus in the midbrain tegmentum.
The interposed nucleus deserves specific attention. Research has identified two distinct neuronal populations within it where vestibular and proprioceptive signals converge. One population carries traditional vestibular signals describing head movement in space. A second population precisely matches vestibular against proprioceptive signals, functionally canceling each other during combined sensory stimulation. This second population encodes body motion in space, not just head motion, providing the reference signal for controlling limb movements throughout the body.
This is the anatomical basis for why PRYT tests two body parts simultaneously. You are stress-testing this integration system. You are asking the interposed nucleus to reconcile proprioceptive input from two ends of the body at once. When the integration fails and an indicator muscle weakens, you have found a fault in that reconciliation process.
The reticular formation is the primary downstream pathway for the postural tone changes you observe after correction. It coordinates eye and head movements while simultaneously regulating postural muscle tone through excitatory and inhibitory pathways throughout the body. Improved proprioceptive input from the upper cervical complex, feeding through the interposed nucleus and into the reticular formation, changes postural tone in the limbs.
That is why the hip opens after you correct the neck. You did not touch the hip. You fixed the reference signal feeding a system that governs tone throughout the body.
Why Roll Is Different
The vestibular nuclei receive convergent input from three sources: the semicircular canals and otolith organs via cranial nerve VIII, upper cervical proprioception via direct cervical afferents, and visual input via the superior colliculus. Research on cervicogenic dizziness shows distinct abnormalities in cervical proprioceptive input that correlate directly with impaired visual-vestibular central integration. The dysfunction is not in the eyes or the vestibular apparatus. It is in the cervical proprioceptive signal corrupting the integration.
The roll test is positive when pelvic and lumbar rotation creates a proprioceptive conflict that the vestibular integration system cannot resolve. When the patient lateralizes their eyes, they are activating the visual righting reflex through the vestibulo-ocular pathway, altering the gain of cervico-vestibular integration. In approximately 70% of positive roll cases, therapy localizing the sacrum alone resolves the indicator muscle weakness. Those are primarily mechanical faults in the sacral proprioceptive network. The remaining 30% represent cases where the visual righting reflex is genuinely integrated into the dysfunction. Those require the full oculobasic protocol because you are dealing with a neurologically different problem, not just a different joint.
Apply
Clear the rocker motion fixation before you test any PRYT pattern. If the primary input station is dysfunctional, your module integration tests are reading through corrupted tissue in the most proprioceptively dense region of the body. Rocker is the prerequisite, not the optional add-on.
When you find a positive pitch, yaw 1, or tilt pattern and make your correction, document the hip range of motion before and after. That change is not a party trick. It is your clinical confirmation that you moved the reference signal feeding the cerebellar comparator. The hip opened because something upstream recalibrated.
The next piece covers what that upstream correction is doing to the vagus nerve, why it matters for every autonomic finding in your recheck, and why the jugular foramen is the most clinically underappreciated piece of anatomy in your practice.
Not a member of the weekly focus?
Join us for the deep dives and all the content of the fundamental Applied Kinesiology course inside the monthly membership of Applied Kinesiology Online!
Cant wait to see you inside of this game we call practice!

